There are many infections and diseases which can be transmitted through our blood. Some of the most common bloodborne infections include HIV, HBV (hepatitis B), and HCV (hepatitis C). One way that HBV, HCV, and HIV transmission can occur is through the use of shared injecting equipment to use substances.
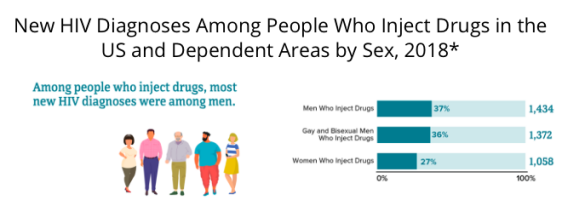
Every time that a person uses a needle to inject drugs, there is a 1 in 160 chance that they could contract HIV. Further, about 10% of all new HIV cases are attributed to the use of shared injecting equipment.
As a result of stigma and fear around talking with medical providers about substance use, many people who use substances don’t share this behavior with their medical provider. As such, they may not be identified as someone that would benefit from increased routine testing and HIV prevention planning.
Thankfully, there are harm reduction programs available to increase HCV, HBV, and HIV prevention efforts. Some of these programs offer new injecting equipment including syringes. Harm reduction is a public health principle designed to decrease the harm associated with these behaviors through education, support, and resources.
If you or someone you know uses substances, here are some things to know about HCV, HBV, and HIV prevention through the lens of harm reduction.
Determine Your Risk Level
First, it is important to understand how HCV and HIV transmission can occur as a result of substance use. HCV is commonly transmitted from one person to another via shared needles or syringes. HCV is a very serious illness that can lead to liver cirrhosis or liver cancer if no treatment is given.
A person with HIV can transmit the virus if their viral load is high enough. The viral load is the measurement of viral cells within their bloodstream.
If a person is taking HIV treatment drugs to suppress their viral load, they cannot transmit it sexually. This means that when a person’s viral load is undetectable (or non-measurable), then they cannot pass it onto someone else sexually.
This is known as U=U regarding HIV transmission. However, people who inject substances may still be able to transmit HIV through shared injecting equipment, and as such they should continue to not share drug preparation or injecting equipment.
If a person’s viral load is high enough (detectable) and they share substance use equipment with another person, it could lead to HIV transmission. This can occur through the use of shared equipment and needles used for substance use, medication injections, piercings, and tattoos.
If you have ever shared needles or injection use equipment for any reason, then you could be at risk for HIV or HCV. It is very important to get tested right away, particularly if you have felt any HIV symptoms such as:
- Fever
- Chills
- Excessive fatigue
- Night sweats
- Muscle ache
- Swollen lymph nodes
- Rash
- Sore throat
- Headache
Connect with Syringe Service Programs
There are programs available all over the country that provide HIV prevention education, resources, and testing for people that use substances. These are programs called harm reduction organizations, syringe service programs, or needle exchange programs.
These programs are welcome and safe spaces where you can safely dispose of used syringes and other supplies so they cannot be reused by others. These organizations also provide new, sterile syringes and supplies. Not only does this aid in HIV prevention, but it also reduces the spread of other bloodborne viruses like hepatitis B and C.
These programs have made a huge difference to significantly lower the number of HIV transmissions throughout the world. In Australia, the number of new HIV cases has decreased by 70% over the past 10 years thanks to the syringe service program.
Many of these organizations also help people who are struggling with substance use disorder to get treatment. Medication Assisted Treatment (MAT) is prescribed medication including methadone or buprenorphine, that can be used to treat opioid use disorder. This and other treatment options help to reduce drug dependence on and the need for substance use equipment and syringes overall.
There are many types of additional harm reduction services available around the world designed to support disease prevention. For instance, safe consumption spaces are sanctioned throughout Canada. People are allowed to legally inject substances in these spaces and are provided with sterile instruments to reduce the risk of HIV transmission. Although this approach is rather controversial, it has helped to lower disease contraction without increasing crime or substance use rates.
You can use sites like HarmReduction.org to find these harm reduction facilities in your area.
Talk to Your Doctor About PrEP
Apart from avoiding practices that put you at risk for HIV transmission, the best way to prevent contraction is to take Pre-Exposure Prophylaxis a.k.a. PrEP. This medication stops HIV from reproducing and spreading in the body after exposure. PrEP must be taken for at least 7 to 21 days for maximum protection and it can be taken indefinitely if you are at risk.
It is important to note the difference between PrEP and PEP. PrEP is taken before exposure to HIV – so you must be HIV negative. PEP is an HIV treatment provided after a confirmed exposure. This medication must be started within the first 72 hours after exposure to be effective for HIV prevention.
So, your first step to taking PrEP or PEP is to get tested by a doctor and discuss your options. This can be quite intimidating, especially since talking about your risk of contracting HIV can be a bit uncomfortable. However, there is nothing more important than protecting your health. If you have used substances or engaged in other behaviors which put you at risk for HIV (such as unprotected sex), you need to talk to your doctor about it.
That’s Where We Come In
Our team here at PrEP Daily is here to help you make that next step. You’ll get connected with a navigator who can answer questions about HIV prevention and taking PrEP. They will also help you find a doctor to prescribe PrEP medication.
You can connect with us online or reach out by calling 1-800-CDC-INFO today!